Using Market Data to Establish Sustainable Physician Compensation Models
Does your healthcare organization rely on the market data that surveys publish to establish physician compensation levels? If so, you are not alone. Many healthcare organizations depend on market data trends to inform their decisions, especially as it relates to establishing physician compensation rates. But, how does this data change each year, and what story does it tell? According to data trends for the past decade, physician compensation metrics have shown a consistent upward trend. With many healthcare organizations relying on survey data alone to make physician compensation decisions, this raises potential questions as to the economic viability of the compensation structure. Meaning, can the healthcare organization afford to pay what the market data reflects?
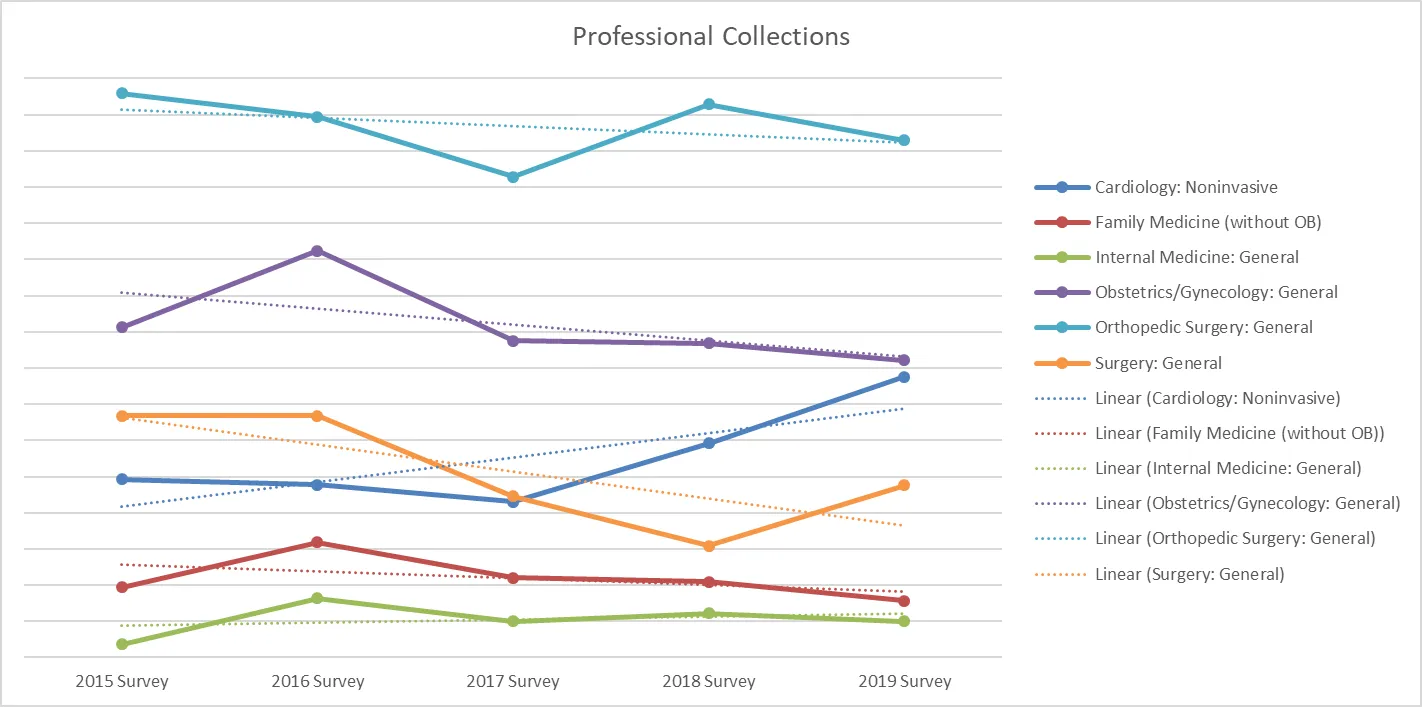
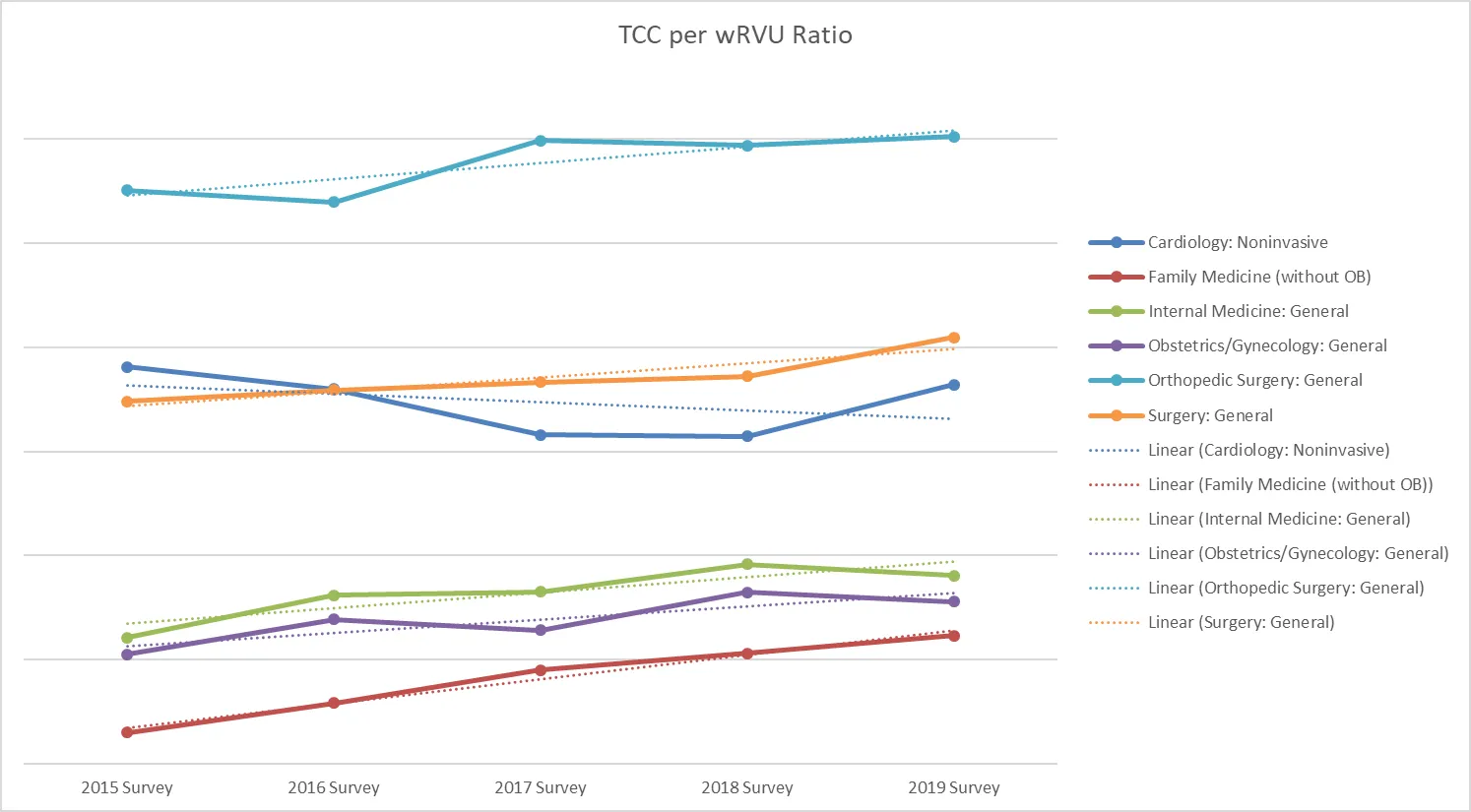
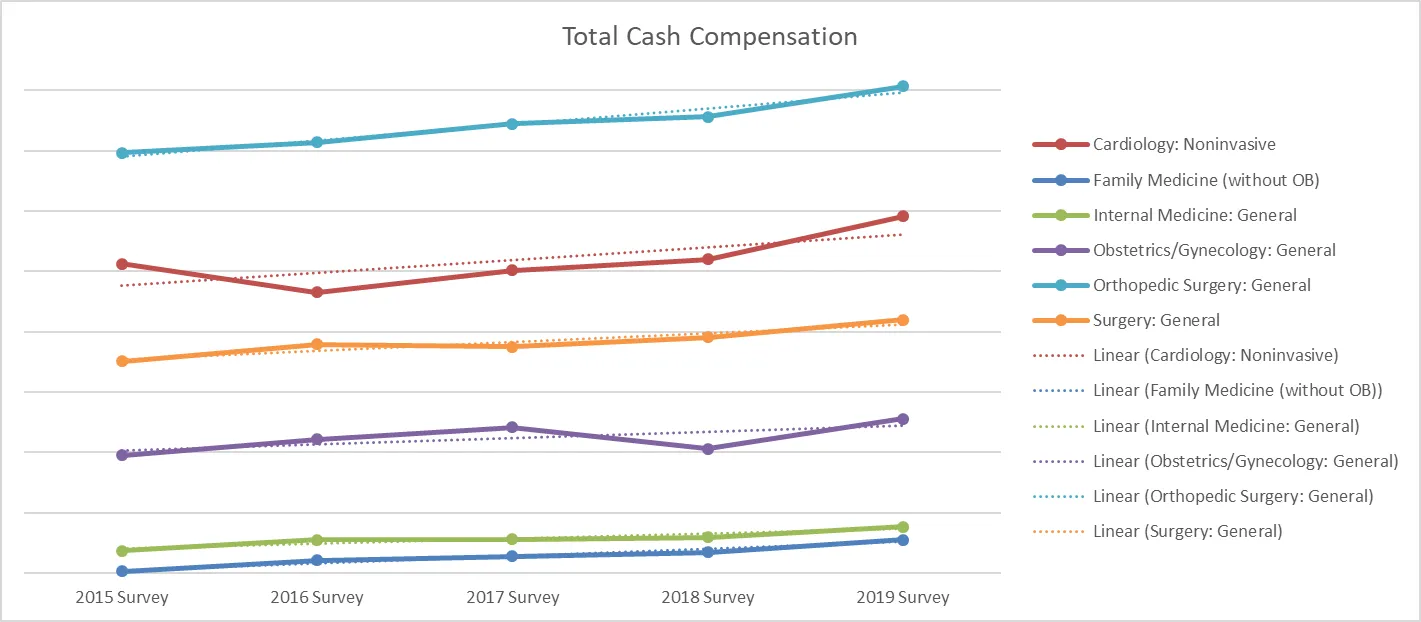
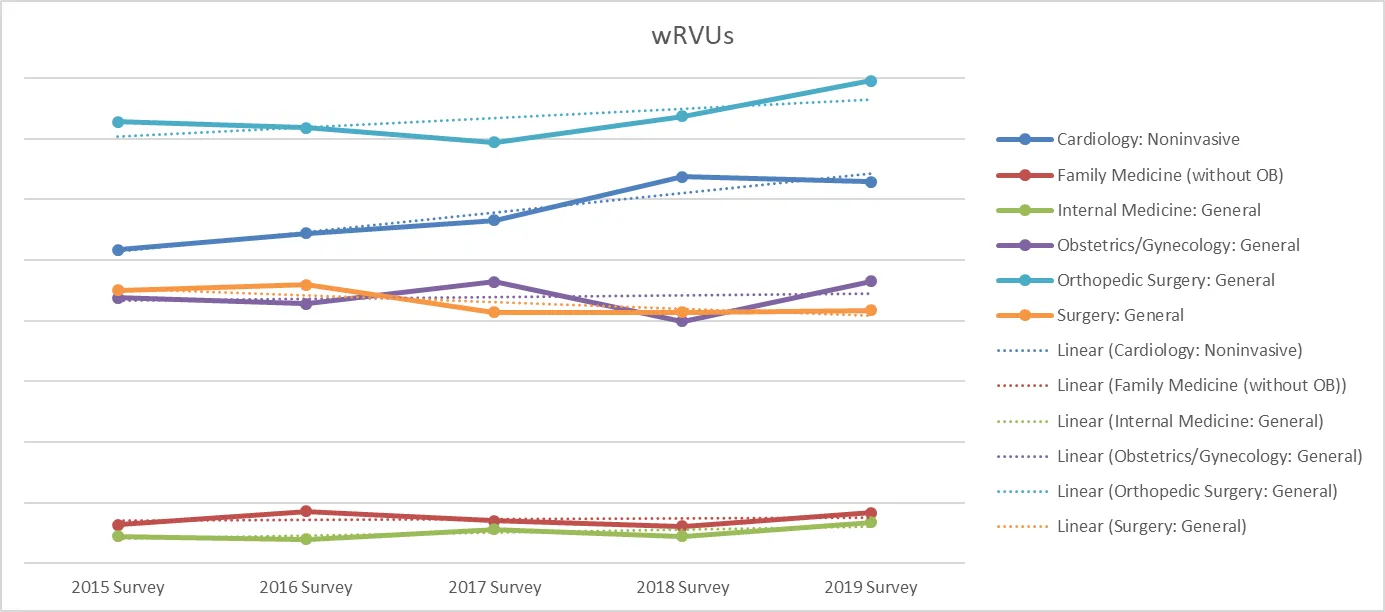
We reviewed the 2019 MGMA Provider Compensation and Productivity Survey Report released in May 2019 and looked at the five-year trend of four key physician compensation and productivity metrics at the median: total cash compensation (TCC), wRVUs, professional collections, and the TCC per wRVU ratio. We focused our review on medical and surgical specialties with a high level of respondents year-over-year.When considering the published market data year-over-year, we see the following:
- a clear upward trend in physician compensation,
- the TCC per wRVU ratio for the majority of specialties, with a less pronounced increase for wRVU productivity data
- while professional collections indicate a clear downward trend for the majority of specialties.
The question is, how many organizations have seen reimbursement increase (or expenses decrease) at the same rates as physician compensation is increasing? Based on the market data, it would appear not many. (Illustrations of all data points are in the charts, below.)Coker is a strong proponent of using market data as a foundation for making physician compensation decisions, while reviewing other key considerations, such as the organization’s actual financial performance, recruitment/retention dynamics, interaction of other components of the compensation model, etc., alongside the data. Ultimately, a solid physician compensation model is one that is both structurally and economically sustainable. Further, contemplating these additional considerations will help ensure such economies exists.
Five-Year Trend Lines for MGMA Provider Compensation and Productivity Survey